Do you snore or sleep with someone that snores? Snoring is annoying and disruptive for the person sleeping with you. Besides being extremely annoying, snoring can be very serious. Frequent loud snoring may be a sign of sleep apnea. Sleep apnea is a common disorder when you have one or more pauses in breathing or short breaths while sleeping. When sleeping, breathing can pause anywhere from ten to twenty seconds and can happen up to one hundred times or more every night. Since the long pauses disrupts your sleep rhythm, you spend more time in light sleep than deep sleep. This sleep deprivation leads to daytime drowsiness, lack of concentration, slow reflexes, and can lead to serious health problems. Over time sleep apnea can cause diabetes, high blood pressure, heart disease, stroke, and weight gain.
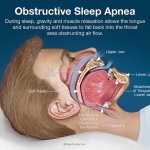
There are different types of sleep apnea. Obstructive Sleep Apnea is the most common. This type of sleep apnea occurs when the soft tissue in the back of your throat relaxes during sleep and blocks the airway.When the airway is blocked, it causes you to snore very loudly. Central Sleep Apnea involves the central nervous system. This occurs when the brain fails to signal the muscles that control breathing. It is a rare type and usually people with this type hardly ever snore. Complex Sleep Apnea is the combination of the other two types of sleep apnea.
If choking or gasping happens after the pause in snoring, it is a major sign that you have sleep apnea. Some people fall asleep very fast during the quiet moments of the day when nothing active is happening. Other common signs and symptoms include: headaches in the morning, lack of memory or learning problems, depression, mood swings, frequent urination, dry mouth, and sore throat.

So how do you know if its just snoring or sleep apnea? If you snore, consult your medical doctor about having a sleep study. There are different ways you and your medical doctor can treat snoring and sleep apnea. We also have a way to help in the dental world. There is a device called the Myerson Sleep Better Appliance also known as EMA. This is a custom made removable appliance that advances the lower jaw and open the bite to help with the restricted airflow during sleep. This appliance helps prevent snoring and relieves the symptoms of sleep apnea. It is also adjustable to patient satisfaction. We provide this option at our office. If you or someone you know snores or has sleep apnea, this appliance may be helpful!






 To help your children stop this habit, try to encourage them with rewards. Provide them with a toy after a certain amount of days they go without sucking their thumb. Mark progress on a calendar where the child can see the progress he/she is making. Most important, no nagging! Children get defensive if the parent is nagging to much about stopping the habit.
To help your children stop this habit, try to encourage them with rewards. Provide them with a toy after a certain amount of days they go without sucking their thumb. Mark progress on a calendar where the child can see the progress he/she is making. Most important, no nagging! Children get defensive if the parent is nagging to much about stopping the habit. they are burning. Sometimes the burning sensation can affect the whole mouth, and not just a certain area. Although Burning Mouth Syndrome can affect anyone, it is most common in middle-aged or older women.
they are burning. Sometimes the burning sensation can affect the whole mouth, and not just a certain area. Although Burning Mouth Syndrome can affect anyone, it is most common in middle-aged or older women. Depending on the cause of BMS, there are medications that can be prescribed to treat the oral candidacies, anxiety, and depression. There are also prescriptions and supplements to relieve dry mouth. Biotene mouth wash is commonly used to treat dry mouth. At home treatment can include sucking on ice chips, drinking plenty of water, avoiding hot and spicy foods, avoiding acidic foods and drinks, and avoiding alcohol and tobacco. If you have any questions about Burning Mouth Syndrome, call our office or physician for more information.
Depending on the cause of BMS, there are medications that can be prescribed to treat the oral candidacies, anxiety, and depression. There are also prescriptions and supplements to relieve dry mouth. Biotene mouth wash is commonly used to treat dry mouth. At home treatment can include sucking on ice chips, drinking plenty of water, avoiding hot and spicy foods, avoiding acidic foods and drinks, and avoiding alcohol and tobacco. If you have any questions about Burning Mouth Syndrome, call our office or physician for more information. The purpose of sealants is to prevent cavities. We recommend children as well as adults to have sealants. As soon as the 6 year molars have fully erupted on your children, you should consider having sealants placed. The 6 year molars (first molars) usually come in between ages 5-7, but that can vary. Later when the 12 year molars erupt, those can also be sealed. The 12 year molars (second molars) usually erupt between ages 8 ½ to 13 years old. Besides, children, anyone who is prone to get cavities should consider getting sealants. Also anyone with deep groves in the biting surfaces of their teeth should consider sealants, since they are hard to keep clean.
The purpose of sealants is to prevent cavities. We recommend children as well as adults to have sealants. As soon as the 6 year molars have fully erupted on your children, you should consider having sealants placed. The 6 year molars (first molars) usually come in between ages 5-7, but that can vary. Later when the 12 year molars erupt, those can also be sealed. The 12 year molars (second molars) usually erupt between ages 8 ½ to 13 years old. Besides, children, anyone who is prone to get cavities should consider getting sealants. Also anyone with deep groves in the biting surfaces of their teeth should consider sealants, since they are hard to keep clean.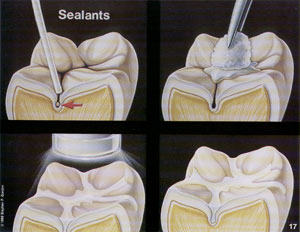 To place a sealant, the tooth must be very dry. Any kind of moisture could prevent the sealant from adhering to the tooth. To ensure dryness, cotton rolls may be placed around your tooth. Next a preparation gel called etch is placed on the tooth. Then that gel will be washed and suctioned (vacuumed) off and the tooth dried by blowing air. Next a bonding agent will be “painted” on the tooth. Then a blue colored ultraviolet (u.v.) light is used to activate the bonding agent. Then the sealant is placed in the groves of the biting surfaces of the tooth. Finally the blue u.v. light is used to make the sealant harden. You may be asked to close your eyes or wear orange colored glasses because it is not good for your eyes to stare at the blue u.v. light.
To place a sealant, the tooth must be very dry. Any kind of moisture could prevent the sealant from adhering to the tooth. To ensure dryness, cotton rolls may be placed around your tooth. Next a preparation gel called etch is placed on the tooth. Then that gel will be washed and suctioned (vacuumed) off and the tooth dried by blowing air. Next a bonding agent will be “painted” on the tooth. Then a blue colored ultraviolet (u.v.) light is used to activate the bonding agent. Then the sealant is placed in the groves of the biting surfaces of the tooth. Finally the blue u.v. light is used to make the sealant harden. You may be asked to close your eyes or wear orange colored glasses because it is not good for your eyes to stare at the blue u.v. light.